Building larger, stronger glutes combines targeted resistance training, strategic nutrition, and consistent effort. Most people see noticeable improvements in glute size and shape within 8–12 weeks when following a structured workout plan with adequate protein intake. However, results depend on your starting point, genetic factors, and adherence to both training and nutrition protocols.
Some individuals observe changes within six weeks, while others require three months of dedicated effort. This comprehensive guide examines glute anatomy, evidence-based training principles, optimal nutrition strategies, lifestyle factors affecting growth, and surgical alternatives for those seeking more dramatic results beyond natural development.
Glute Muscle Anatomy: Building Your Glutes Effectively
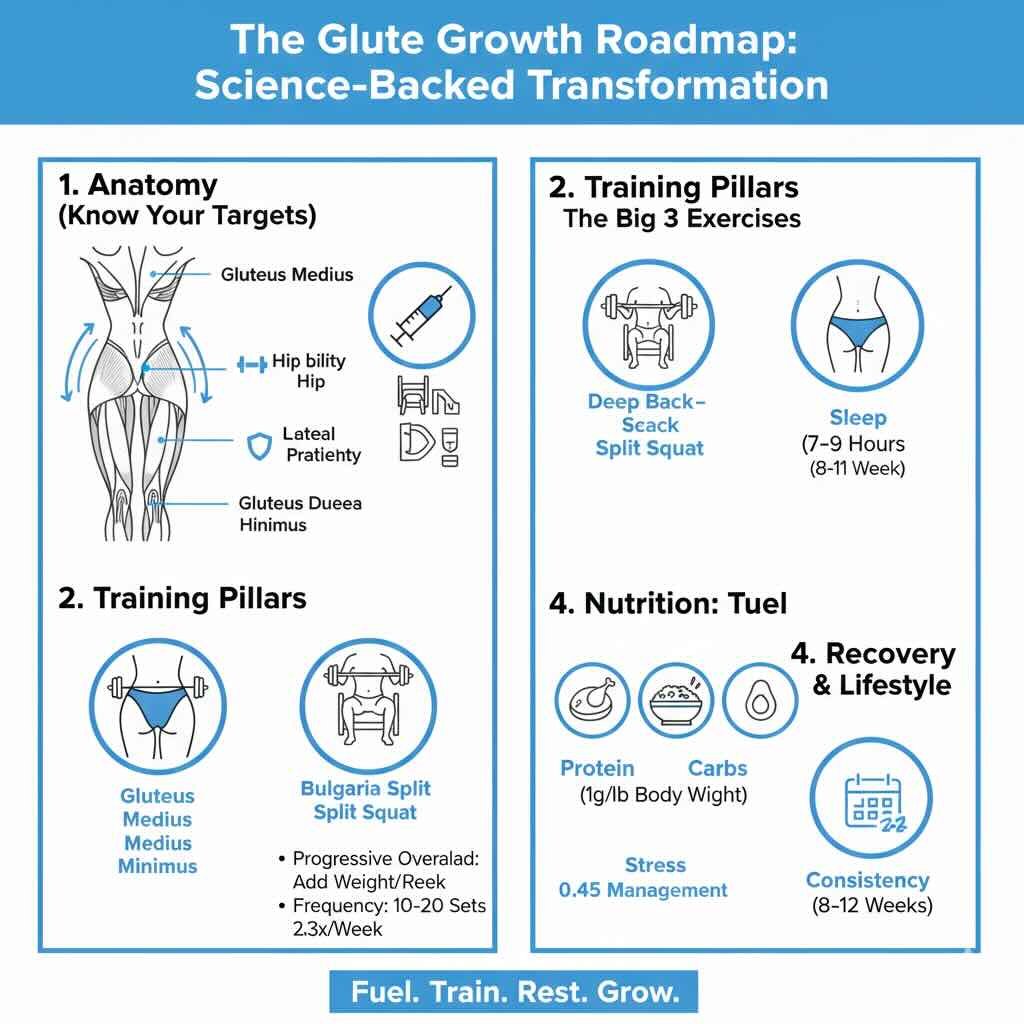
The gluteal muscles consist of three distinct layers working together to control hip movement and provide stability. Understanding each muscle’s role helps you target them effectively during training.
- Gluteus Maximus: The largest and most superficial muscle drives hip extension and external rotation. It provides the primary contributor to overall butt volume and shape. It activates heavily during squats, hip thrusts, and deadlifts.
- Gluteus Medius: Located on the outer upper portion of the buttocks, this muscle controls hip abduction and pelvic stabilization. It creates the rounded “shelf” appearance on the upper-outer glutes. Weakness leads to hip drops during single-leg movements.
- Gluteus Minimus: The smallest muscle lies beneath the medius and assists with hip abduction and internal rotation. It contributes to balanced development and maintains proper pelvic alignment during walking and running.
The gluteal muscles generate power for running and jumping, support the lower back, and enable basic activities like walking and climbing stairs. Modern sedentary lifestyles create a significant obstacle. Extended sitting causes gluteal muscles to become underactive, allowing quadriceps and hamstrings to dominate during movement.
This muscular imbalance limits glute growth potential and increases injury risk. Individual results depend on genetic factors including pelvic structure, natural fat distribution, and muscle fiber composition. Targeted training enhances your natural body architecture rather than transforming it into a different shape category.
Someone starting with a flat butt can develop noticeable roundness and projection. Those with naturally rounded contours can increase size and definition.
Evidence-Based Strength Training to Make Your Butt Bigger
Three critical factors maximize muscle adaptation. These include systematically increasing training demands (progressive overload), managing workout volume and frequency appropriately, and establishing strong neural connections with the glute muscles during exercise.
Progressive Overload: The Foundation to Build a Bigger Booty
Progressive overload forms the foundation of muscle growth. Without consistently increasing the training stimulus, the body has no reason to build additional muscle tissue. The most straightforward approach involves adding weight to exercises over time.
A trainee might start hip thrusts with 95 pounds and gradually work up to 225 pounds over several months. This creates mechanical tension that forces the glutes to adapt by growing larger and stronger.
Additional progression strategies include:
- Increasing repetitions: Once you complete 12 reps of Bulgarian split squats with a given weight, aim for 15 reps before adding load
- Adding sets: Progressing from 3 to 4 sets increases total training volume
- Reducing rest periods: Shorter breaks between sets intensify the metabolic demand
- Improving range of motion: Deeper squats engage more muscle fibers
- Slowing movement tempo: Extending the lowering portion to 3–4 seconds while maintaining constant tension maximizes muscle fiber recruitment, particularly benefiting Romanian deadlifts and Bulgarian split squats
- Adding pauses: Holding at peak contraction points for 1–2 seconds before beginning the next repetition increases time under tension
When hands fatigue before glutes during exercises like deficit lunges or Romanian deadlifts, lifting straps transfer the load directly to the target muscles. This allows you to handle weights that appropriately challenge the glutes without premature set termination.
Training Volume and Frequency to Get Bigger, Stronger Glutes
Training volume refers to the total amount of work performed, typically measured in sets per muscle group per week. Research suggests 10–20 challenging sets per week produces optimal growth for most intermediate trainees. Beginners should start with 8–12 sets weekly to allow proper recovery and adaptation.
Start with a single well-executed set of each exercise to establish proper movement patterns. Gradually advance to two sets, then three, eventually reaching four sets as strength improves. Advanced trainees may handle up to 36 weekly sets across three categories: vertical hip extension, horizontal hip extension, and abduction exercises.
This higher volume becomes manageable when exercises target different movement patterns, preventing excessive stress accumulation. Training frequency determines how often glutes are trained each week. Most people achieve best results training glutes 2–3 times weekly, allowing 48–72 hours between sessions for recovery.
This rest period enables protein synthesis and tissue repair—essential processes for muscle growth that occur outside the gym. An effective weekly structure follows a lower-upper-lower-upper-lower pattern, distributing three dedicated glute sessions throughout the week with upper body training days positioned between them.
For optimal hypertrophy results, perform each exercise for 6–12 repetitions at approximately 75–85% of one repetition maximum. Complete 3–5 sets per exercise with 60–90 second rest intervals between sets. Women frequently express concern about developing excessively muscular glutes through resistance training.
Female physiology naturally limits muscle mass accumulation due to lower testosterone levels. Higher repetition ranges of 12–15 reps per set emphasize muscle tone and firmness. Substantial hypertrophy remains physiologically difficult for most women regardless of training approach.
Achieving measurable glute growth requires sufficient load that challenges muscles beyond simple metabolic stress.
The Best Exercises for Building Glutes
Achieving a bigger butt requires targeting all three gluteal muscles through compound movements that emphasize hip extension and progressive overload. Electromyography testing reveals that vertical hip extension movements like squats preferentially activate the lower portion of the gluteus maximus. Horizontal movements target different regions, suggesting you should include both types for comprehensive development.
1. Hip Thrusts: The King of Glute Exercises
The hip thrust produces among the highest glute activation levels of any exercise according to EMG studies, with research showing significantly greater gluteus maximus recruitment compared to squats. It isolates hip extension while minimizing quad involvement. Proper setup requires the upper back positioned on a bench with feet flat and knees at 90 degrees at the top position.
2. Squats and Variations for Vertical Hip Extension
The back squat remains a foundational movement for glute development when performed with adequate depth. Breaking parallel activates the glutes maximally during the concentric portion of the lift. Stance width significantly affects glute recruitment.
3. Lunges and Split Squats for Unilateral Development
Walking lunges challenge balance while targeting each glute independently. The forward stride requires hip flexor flexibility and activates the trailing leg’s glute through a stretched position. The Bulgarian split squat elevates the rear foot on a bench, creating an intense stretch in the front leg’s glute.
Nutrition
Growing bigger glutes demands eating in a caloric surplus to provide muscles with fuel for recovery and growth. The caloric surplus should remain modest—typically200–300 calories above maintenance levels. This controlled approach supports muscle growth while minimizing unnecessary fat accumulation.
Eating substantially beyond this range directs excess calories toward fat storage rather than muscle development. This potentially obscures the glute definition achieved through training. Individuals seeking to reduce overall buttock size rather than increase it should focus on creating a caloric deficit while maintaining protein intake to preserve muscle tissue.
Glute-specific exercises combined with calorie restriction reduce the subcutaneous fat layer covering the gluteal muscles. This results in a firmer, smaller appearance.
Protein: The Building Block of Muscle
Protein serves as the primary building block for muscle development. Most individuals should consume approximately 1 gram of protein per pound of body weight daily. When actively building muscle mass, nutritionists recommend that protein comprise 25–35% of total daily caloric intake to optimize tissue synthesis and recovery.
High-quality protein sources include chicken breast, salmon (provides omega-3 fatty acids that support recovery), and eggs (deliver all essential amino acids needed for muscle synthesis). Greek yogurt combines high protein content with probiotics for digestive health. Cottage cheese offers slow-digesting casein for sustained protein delivery.
Additional sources include lean beef, almonds and peanut butter (provide plant-based protein plus healthy fats), and quinoa (stands out among grains as a complete protein source suitable for vegetarian diets). Lentils provide 9 grams per half-cup serving. Chia seeds offer amino acids and omega-3 fatty acid content.
Carbohydrates, Fats, and Training Fuel
Complex carbohydrates like brown rice, quinoa, and sweet potatoes provide energy for intense glute training sessions. Carbohydrates stimulate insulin production, creating an anabolic environment that promotes muscle protein synthesis. Consuming carbohydrates around training sessions maximizes this effect, helping shuttle nutrients into muscle cells for growth and recovery.
Training with adequate pre-workout fuel proves particularly important for glute hypertrophy. While training in a fasted state may benefit fat reduction goals, consuming carbohydrates 1–2 hours before resistance sessions provides the glycogen necessary for maximal training intensity. This also supports muscle protein synthesis.
Healthy fats from sources such as avocados, nuts, nut butters, and olive oil support hormone production necessary for muscle growth.
Daily Macronutrient Targets:
- Protein: 1g per lb body weight (chicken, salmon, eggs, Greek yogurt)
- Carbohydrates: 2–3g per lb body weight (brown rice, quinoa, oats, sweet potatoes)
- Fats: 0.4–0.5g per lb body weight (avocados, nuts, olive oil, fatty fish)
Lifestyle Factors That Support or Hinder Growth
Muscle growth occurs during rest periods, not during workouts. The glutes need adequate recovery time between training sessions to repair and grow larger.
Sleep: The Ultimate Recovery Tool
Sleep plays a critical role in building bigger glutes. During deep sleep, the body releases growth hormone that facilitates muscle repair and development. Adults should aim for 7–9 hours of quality sleep per night.
Optimizing sleep quality enhances recovery effectiveness. Keep bedroom temperature between 60–67°F to promote deeper sleep cycles. Establish consistent bedtime routines.
Expose yourself to morning sunlight to regulate circadian rhythm. Discontinue caffeine consumption 8–10 hours before sleep. Reserve your bed exclusively for sleep to strengthen the mental association between bed and rest.
Recovery, Stress Management, and Consistency
Active recovery techniques enhance glute development. Light stretching, foam rolling, and walking improve blood flow to muscles without causing additional stress. These practices reduce soreness and prepare the glutes for subsequent training sessions.
Stress management protects muscle gains. Elevated cortisol levels from chronic stress can interfere with muscle protein synthesis and promote fat storage. Psychological stress directly impacts body composition through elevated cortisol, which can interfere with fat distribution patterns and impede glute development.
Managing mental health supports physical training goals. This makes stress reduction practices like meditation, yoga, or breathing exercises essential components of any body transformation program. Consistency determines success in building glutes.
Training the glute muscles 2–3 times per week with progressive overload produces measurable results over time. Alcohol consumption should be limited when pursuing glute growth. Alcohol impairs protein synthesis and disrupts sleep quality, both critical factors for muscle development.
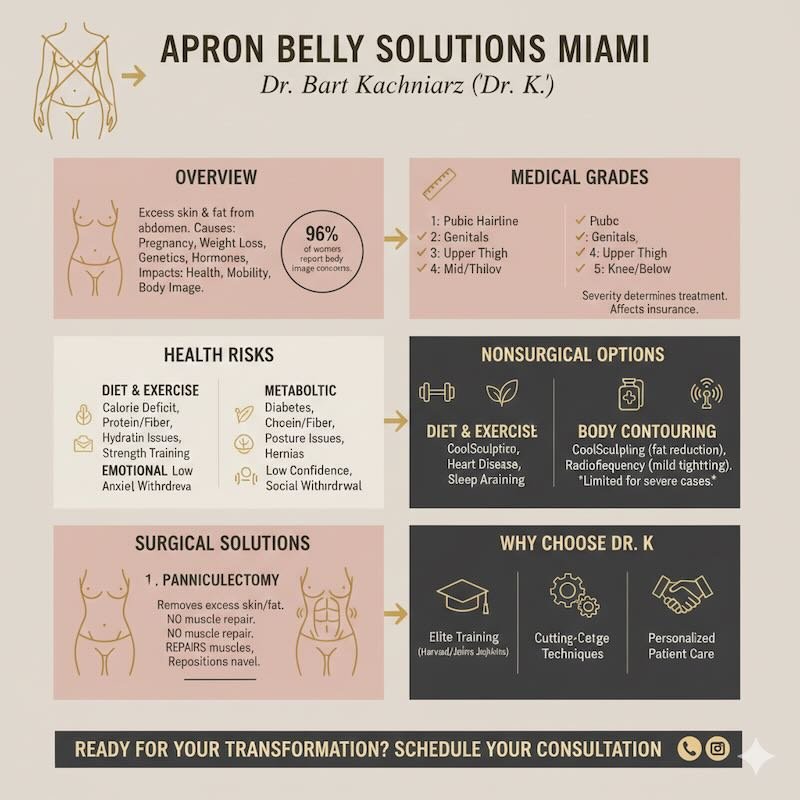
What to do When Exercise is not enough?
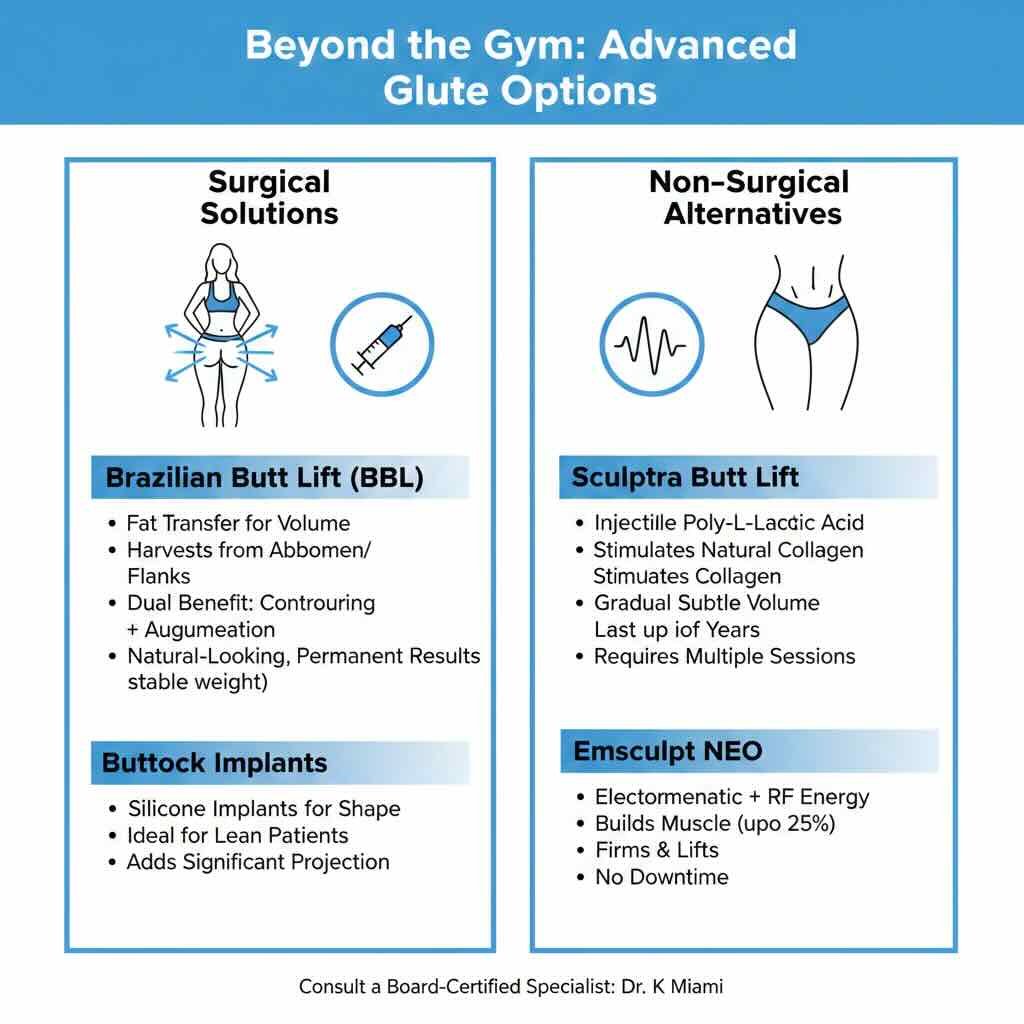
Exercise-based development enhances existing glute architecture rather than fundamentally altering natural shape categories. Dramatic shape transformation beyond one’s genetic template typically requires surgical intervention.
This should only occur after natural training approaches have been exhausted.
Get A Bigger Butt through A BBL
Surgical butt enhancement delivers the most significant and lasting results for patients seeking substantial size increases. The Brazilian Butt Lift combines liposuction with fat transfer, simultaneously contouring donor areas while enlarging the buttocks. This approach creates natural-looking results since the body accepts its own fat tissue.
A Brazilian Butt Lift enhances buttock size and shape by harvesting excess fat from areas where it accumulates naturally. Surgeons identify donor sites such as the abdomen, flanks, thighs, or back where fat removal will improve body contours. This creates a dual benefit by slimming donor areas while augmenting the buttocks.
The liposuction phase begins with injecting tumescent fluid into donor sites to facilitate fat removal and minimize bleeding. Surgeons use specialized cannulas to carefully extract fat cells while preserving their viability for transfer. Once harvested, the fat undergoes purification to remove blood, oil, and damaged cells through centrifugation or filtration.
The surgeon then injects the purified fat into multiple layers of the buttock tissue using small cannulas. Strategic placement in different depths and locations ensures even distribution and maximizes fat survival. Surgeons typically overfill the treatment area by 20–30% because not all transferred fat cells establish a blood supply.
The body naturally reabsorbs some fat during the healing process. Patients must maintain stable weight after surgery because significant weight fluctuations affect the transferred fat cells.
Non-Surgical Options
Sculptra butt lift involves injecting poly-L-lactic acid to stimulate collagen production gradually. This non-surgical option requires multiple treatment sessions spaced weeks apart. Results appear subtly over several months and can last up to two years.
The procedure suits patients seeking modest enhancement without surgery or downtime. However, Sculptra provides limited volume compared to surgical options and requires maintenance treatments.
Emsculpt NEO represents an FDA-approved non-surgical technology that combines electromagnetic energy with body contouring principles. Clinical studies demonstrate up to 25% muscle enhancement in treated areas. Patients report improved firmness and lifted appearance.
The treatment requires no anesthesia or recovery time.
Ready to Transform Your Confidence?
Whether you’re considering a Brazilian Butt Lift, buttock implants, or want to explore which option is right for you, Dr. Bart Kachniarz at Dr. K Miami brings Harvard Medical School and Johns Hopkins Hospital training to every procedure. At Dr. K Miami’s boutique plastic surgery practice, you’ll receive personalized care from consultation through recovery. The focus is on natural-looking results that complement your unique body shape.
source https://drkmiamiplasticsurgery.com/how-to-get-a-bigger-butt-evidence-based-glutes